Introduction
Medicare Advantage (MA)—also known as Medicare Part C—is a rapidly growing segment of the U.S. healthcare system, offering beneficiaries an alternative to traditional Medicare by providing private plan options that often include additional benefits. As of 2023, over 45 million Americans are enrolled in Medicare Advantage plans, representing more than 45% of all Medicare beneficiaries, with projections indicating continued growth.
While MA plans have expanded access, introduced innovative care models, and often deliver higher member satisfaction, they also face significant challenges in supporting the health of their enrollees effectively. These challenges include managing complex chronic conditions, addressing social determinants of health, ensuring equitable access, and reducing disparities.
The Centers for Medicare & Medicaid Services (CMS) plays a critical role in shaping the landscape of Medicare Advantage through regulations, quality measures, and payment policies. However, there remains substantial room for CMS to enhance its support to maximize health outcomes for beneficiaries.
This article explores how CMS can better support health in Medicare Advantage by examining current limitations and proposing actionable strategies grounded in healthcare innovation, policy reform, and equity-focused initiatives.
The Current Landscape of Medicare Advantage
Growth and Significance
Medicare Advantage has experienced exponential growth over the past decade. From about 16 million enrollees in 2013, it has more than doubled, driven by favorable policy incentives, supplemental benefits, and consumer demand for comprehensive coverage.
Model of Care
MA plans often employ capitated payments to deliver a broad array of services, including preventive care, chronic disease management, and ancillary benefits such as vision, dental, and fitness programs. Many plans also incorporate care coordination models like Patient-Centered Medical Homes (PCMHs) and Accountable Care Organizations (ACOs).
Challenges in Supporting Member Health
Despite these innovations, several systemic challenges hinder the full realization of health support:
- Fragmented Care Delivery: Variability in provider engagement and coordination.
- Limited Addressing of Social Determinants: Insufficient integration of social needs into care plans.
- Quality Measurement Gaps: Existing metrics may not fully capture health improvement efforts.
- Disparities: Enrollees from minority and socioeconomically disadvantaged groups often experience poorer outcomes.
- Data and Technology Limitations: Fragmented data systems impede comprehensive health management.
Opportunities for CMS to Better Support Health in Medicare Advantage
1. Enhancing Quality Measurement and Outcome Tracking
Current State: CMS currently uses a range of star ratings, including metrics on preventive services, chronic condition management, hospital readmissions, and patient satisfaction. However, these measures may not fully reflect health support activities, especially social determinants and functional status.
Recommendations:
- Develop and Expand Metrics on Functional Status and Social Needs: Incorporate measures that assess mobility, cognitive function, social engagement, and social risk factors.
- Integrate Patient-Reported Outcomes (PROs): Allow beneficiaries to directly report on health status, mental health, and social well-being.
- Use Real-World Data and Wearables: Leverage data from electronic health records (EHRs), claims, and wearable devices to assess health trajectories.
2. Strengthening Payment and Incentive Structures
Current State: CMS’s capitation payments and quality bonuses incentivize certain activities but may not sufficiently reward proactive health support efforts.
Recommendations:
- Introduce Value-Based Payments for Social Determinants of Health: Provide financial incentives to plans that effectively address housing, transportation, food security, and social isolation.
- Reward Functional and Social Outcomes: Adjust payments based on improvements in functional status and social engagement, not solely clinical metrics.
- Support Capitated Payments for Care Management: Increase funding for intensive care management, especially for high-risk populations.
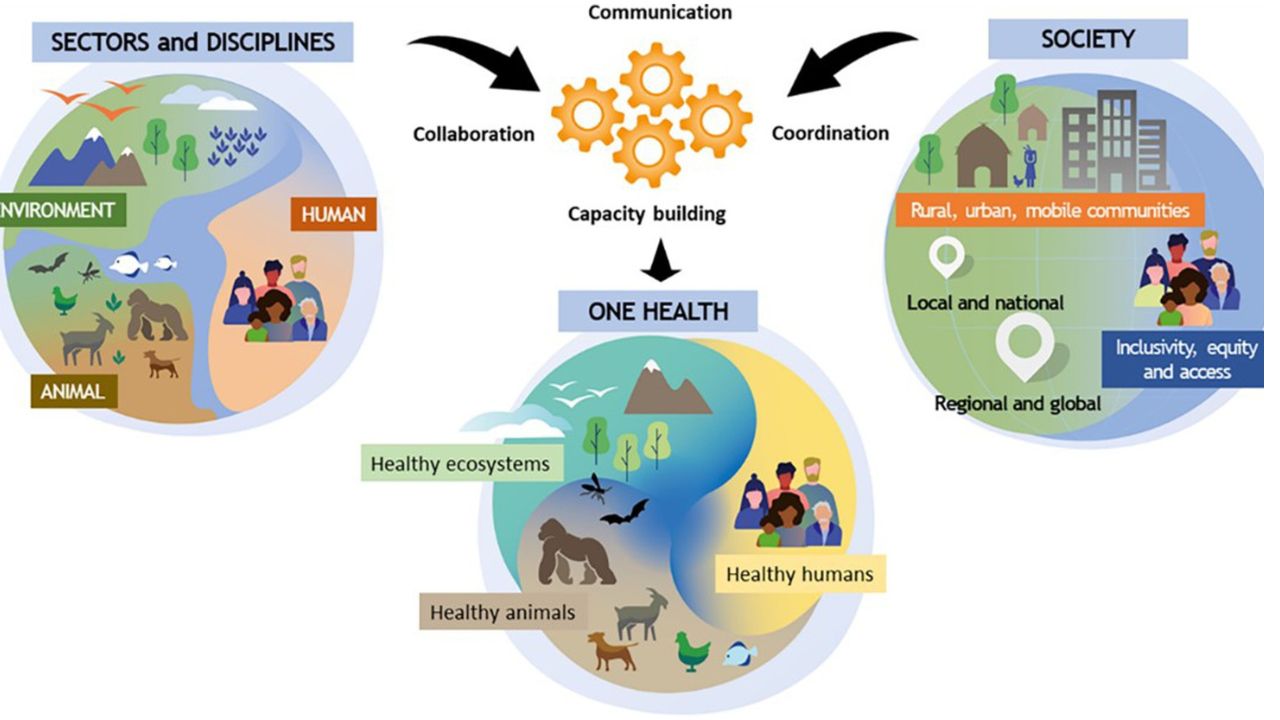
3. Promoting Integrated and Holistic Care Models
Current State: Many MA plans are experimenting with integrated care, but broader CMS support and standardization are needed.
Recommendations:
- Expand Support for Care Coordination Models: Offer technical assistance and funding for implementing models like PCMHs, ACOs, and community-based partnerships.
- Encourage Cross-Sector Collaboration: Facilitate partnerships between healthcare providers, social services, housing agencies, and community organizations.
- Facilitate Data Sharing and Interoperability: Invest in infrastructure that allows seamless sharing of health and social data among providers and plans.
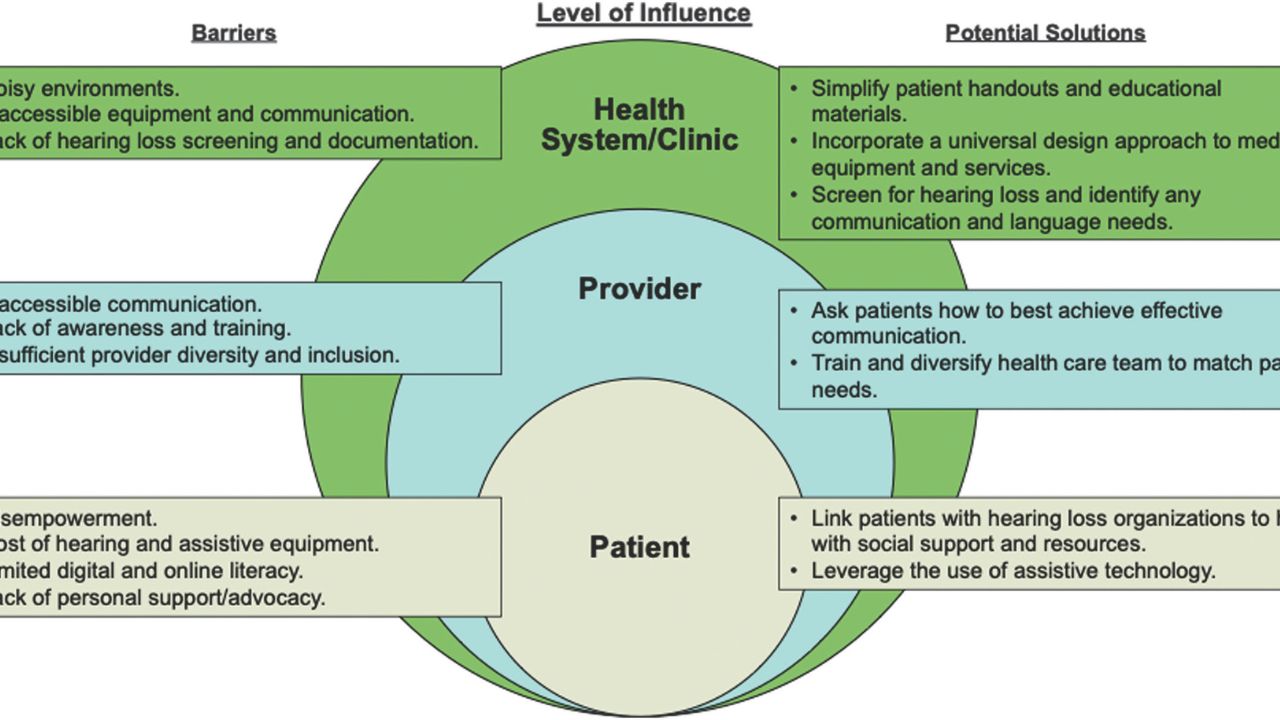
4. Addressing Health Disparities and Promoting Equity
Current State: Disparities persist across racial, ethnic, socioeconomic, and geographic lines.
Recommendations:
- Implement Equity-Focused Quality Measures: Develop metrics that specifically track disparities in access, utilization, and outcomes.
- Allocate Funding for Targeted Interventions: Support programs tailored to underserved communities.
- Mandate Diversity and Cultural Competency Training: Require plans to incorporate culturally sensitive care practices.
- Incentivize Plan Enrollment and Retention in Disadvantaged Areas: Use geographic and socioeconomic factors in payment adjustments.
5. Leveraging Data and Technology
Current State: Data silos and limited analytics hamper comprehensive support.
Recommendations:
- Invest in Interoperable Data Infrastructure: Facilitate real-time data exchange across providers, plans, and social service agencies.
- Use Predictive Analytics: Identify at-risk beneficiaries before crises occur.
- Expand Utilization of Telehealth and Digital Tools: Support remote monitoring, virtual care, and digital literacy programs.
6. Supporting Beneficiary Engagement and Education
Current State: Engagement varies, and many beneficiaries lack understanding of available services.
Recommendations:
- Develop Personalized Care Plans: Use data to tailor support and empower beneficiaries.
- Enhance Educational Resources: Provide clear, culturally appropriate information about benefits and health management.
- Incentivize Preventive and Self-Management Activities: Offer rewards or recognition for participation in wellness programs.
7. Streamlining Regulatory and Policy Frameworks
Current State: Regulations can be complex and sometimes inhibit innovation.
Recommendations:
- Simplify and Harmonize Rules: Reduce administrative burdens on plans and providers.
- Pilot Innovative Programs: Use CMS Innovation Center pathways to test new support models.
- Facilitate Flexibility in Benefit Design: Allow plans to customize offerings based on local needs.
Strategic Initiatives for CMS: A Roadmap
Based on these opportunities, CMS can pursue a comprehensive strategy to improve health support in Medicare Advantage:
A. Establish a Holistic Quality and Support Framework
- Develop a new set of metrics that balance clinical outcomes, functional status, social determinants, and beneficiary experience.
- Incorporate these metrics into star ratings and payment adjustments to create stronger incentives.
B. Expand Funding and Technical Assistance
- Invest in community-based programs and social care integration.
- Provide technical assistance to plans implementing innovative models.
C. Foster Cross-Sector Partnerships
- Formalize collaborations between healthcare, social services, housing, transportation, and community organizations.
- Enable shared data platforms to coordinate care and address social needs.
D. Pilot and Scale Innovative Models
- Use CMS Innovation Center programs to test approaches like social risk-adjusted payments, digital health tools, and community health worker programs.
- Evaluate outcomes rigorously and scale successful initiatives.
E. Prioritize Equity and Disparity Reduction
- Set clear goals and accountability metrics.
- Support targeted outreach and culturally competent care.
F. Enhance Data Infrastructure and Analytics
- Promote interoperability standards.
- Use big data and AI to proactively manage health risks.
Challenges and Considerations
While these strategies hold promise, several challenges must be addressed:
- Data Privacy and Security: Ensuring beneficiary data is protected.
- Resource Allocation: Balancing investments between clinical and social support.
- Equity in Implementation: Preventing plans from cherry-picking healthier populations.
- Provider and Plan Readiness: Ensuring capacity for new care models and data systems.
Overcoming these obstacles requires collaborative planning, stakeholder engagement, and phased implementation.
Conclusion
Medicare Advantage is a vital component of the U.S. healthcare system, offering opportunities to deliver comprehensive, person-centered care. However, to truly support health—especially among vulnerable populations—CMS must go beyond traditional payment and quality measures and embrace a holistic, integrated approach.
By expanding and refining quality metrics, incentivizing social and functional health support, fostering cross-sector partnerships, leveraging technology, and prioritizing health equity, CMS can significantly enhance the capacity of MA plans to improve health outcomes. These efforts will not only benefit beneficiaries but also serve as a model for health system transformation nationally.
The path forward involves bold policy initiatives, strategic investments, and stakeholder collaboration. With dedicated leadership and innovative thinking, CMS can transform Medicare Advantage into a true vehicle for supporting health—mind, body, and social well-being—for millions of Americans.