Introduction
Healthcare is a fundamental pillar of society, encompassing the prevention, diagnosis, treatment, and management of illness and disease. Over the decades, the business of healthcare has evolved dramatically from traditional fee-for-service models to complex, multi-layered systems driven by technological innovation, policy changes, and shifting consumer expectations. Understanding the business side of healthcare involves examining its economic structures, stakeholder roles, financial mechanisms, market dynamics, challenges, and future trends. This comprehensive analysis aims to provide a detailed exploration of the business of health care, offering insights into how healthcare organizations operate, innovate, and adapt in a rapidly changing environment.
1. Historical Context and Evolution of Healthcare Business Models
1.1 Early Healthcare Systems
Historically, healthcare was primarily delivered through community-based or familial care, with limited formalized institutions. As medical knowledge advanced, hospitals and clinics emerged, often financed through charitable donations, government funding, or out-of-pocket payments by patients.
1.2 The Rise of Fee-for-Service Models
In the 20th century, fee-for-service (FFS) became the dominant payment model, where providers billed for each service rendered. While incentivizing volume, FFS often led to unnecessary procedures and escalating costs.
1.3 Shift Toward Managed Care
In response to rising costs, managed care organizations (MCOs), such as Health Maintenance Organizations (HMOs) and Preferred Provider Organizations (PPOs), gained prominence in the late 20th century. These models emphasized cost containment, preventive care, and provider networks.
1.4 The Move to Value-Based Care
Recently, there has been a paradigm shift toward value-based care, where reimbursement is tied to patient outcomes, quality, and efficiency. This transition aims to improve health outcomes while controlling costs.
2. Key Stakeholders in the Healthcare Business
2.1 Patients and Consumers
Patients are at the center of the system, increasingly acting as informed consumers making choices based on quality, cost, and convenience.
2.2 Providers
Includes physicians, hospitals, clinics, and alternative care providers. Their primary role is delivering care, but they also operate as businesses with revenue streams, costs, and strategic priorities.
2.3 Payers
Insurance companies, government programs (Medicare, Medicaid), and employers who finance healthcare services. Payers negotiate prices, manage benefits, and influence provider behavior.
2.4 Pharmaceutical and Medical Device Companies
Innovators and manufacturers of drugs and medical technologies, vital for treatment but also significant drivers of healthcare costs.
2.5 Policy Makers and Regulators
Government agencies and legislators who establish rules, reimbursement policies, and standards affecting healthcare delivery and financing.
2.6 Technology and Data Firms
Providers of electronic health records (EHRs), telehealth, AI, and analytics that enable modern healthcare management.
3. Financial Mechanics of Healthcare
3.1 Revenue Streams
- Fee-for-Service Payments: Direct payments for each service.
- Capitation: Fixed amount per patient regardless of services provided.
- Bundled Payments: Single payments covering a range of services.
- Value-Based Payments: Incentives linked to quality and outcomes.
3.2 Cost Structures
- Direct Costs: Salaries, medical supplies, equipment, pharmaceuticals.
- Indirect Costs: Administrative expenses, facility overheads, compliance costs.
- Capital Costs: Investments in infrastructure, technology.
3.3 Pricing and Reimbursement
Pricing varies by provider, service type, payer contracts, and regulations. Reimbursement rates are often determined by government programs or negotiated insurance contracts.
3.4 Profitability and Financial Sustainability
Healthcare organizations aim to balance revenues and costs, but many operate with tight margins, especially in public or nonprofit sectors, relying on subsidies and grants.
4. Market Dynamics and Competition
4.1 Consolidation and Mergers
Hospitals, provider groups, and insurers often merge to increase bargaining power, reduce costs, and expand market share.
4.2 Entry of New Competitors
Tech companies, retail clinics, telehealth providers, and direct-to-consumer brands are disrupting traditional models.
4.3 Consumer-Driven Market
Patients increasingly seek transparency, convenience, and personalized care, influencing provider offerings.
4.4 Geographic and Demographic Factors
Market size, population health trends, and socioeconomic factors shape healthcare demand and supply.
5. Challenges Facing the Healthcare Business
5.1 Rising Healthcare Costs
Healthcare expenditure accounts for a significant portion of GDP worldwide, driven by aging populations, technological advancements, and high drug prices.
5.2 Inequities and Access
Disparities in healthcare access and outcomes pose ethical and economic challenges, often linked to socioeconomic status and geographic location.
5.3 Regulatory Complexity
Healthcare is heavily regulated, with policies affecting reimbursement, licensing, data privacy, and quality standards.
5.4 Technological Disruption
Rapid innovation demands substantial investment and adaptation, but also introduces risks related to cybersecurity, interoperability, and obsolescence.
5.5 Workforce Shortages
Aging providers, burnout, and shortages of trained healthcare workers threaten service delivery.
6. Innovations and Trends Shaping the Business of Healthcare
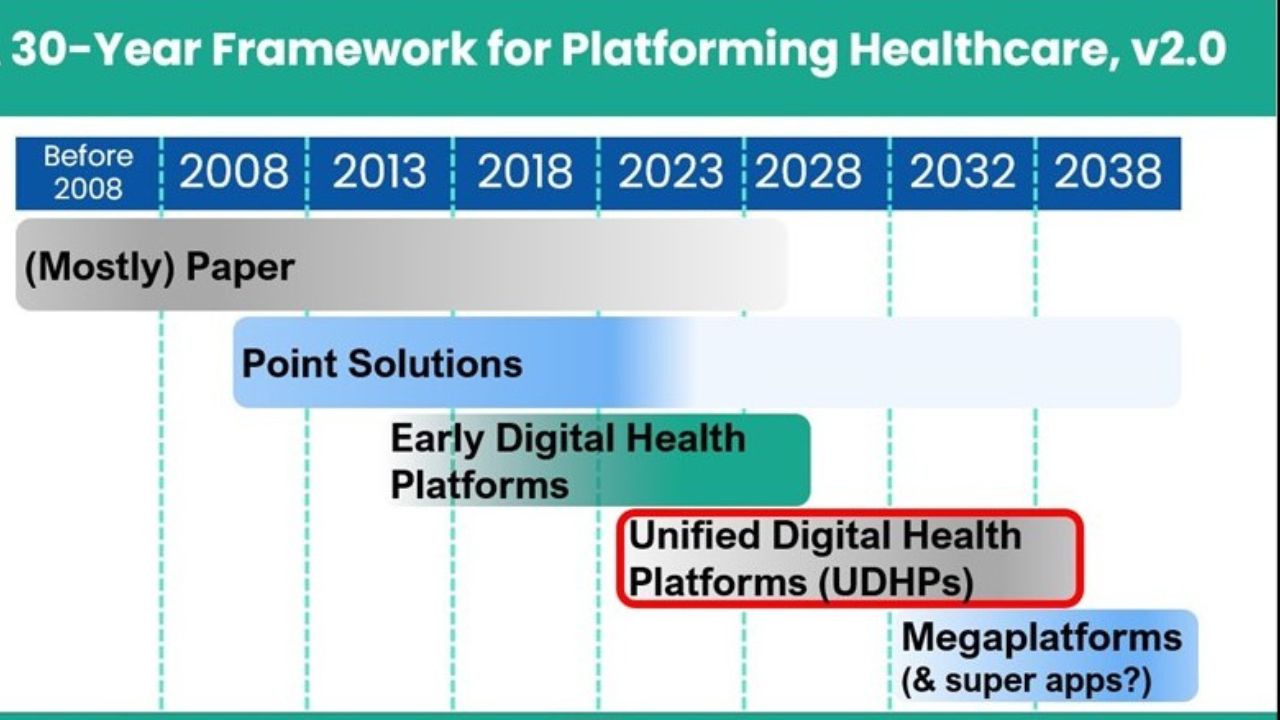
6.1 Digital Health and Telemedicine
Remote consultations, mobile health apps, and remote monitoring improve access and efficiency.
6.2 Artificial Intelligence and Data Analytics
AI enables predictive analytics, personalized medicine, and operational efficiencies.
6.3 Value-Based Care and Payment Models
Incentivizing quality over quantity aims to improve outcomes and reduce unnecessary procedures.
6.4 Patient Engagement and Experience
Digital tools empower patients, fostering adherence, satisfaction, and better health management.
6.5 Precision Medicine
Genomics and biomarker-driven therapies personalize treatment, but also increase costs and complexity.
7. Strategic Considerations for Healthcare Organizations
7.1 Navigating Regulatory Environments
Staying compliant with evolving laws and policies is critical.
7.2 Investing in Technology
Adopting EHRs, telehealth, and data analytics can enhance operational efficiency and patient care.
7.3 Emphasizing Quality and Outcomes
Focusing on evidence-based practices and patient satisfaction improves reputation and reimbursement.
7.4 Diversification and Integration
Vertical and horizontal integration can create more comprehensive care pathways and revenue streams.
7.5 Building Strategic Partnerships
Collaborations with technology firms, payers, and community organizations expand reach and capabilities.
8. The Future of the Business of Healthcare
8.1 Emphasis on Preventive and Population Health
Shifting focus from reactive treatment to proactive health management reduces costs and improves outcomes.
8.2 Global Health Markets
Emerging economies present growth opportunities, but also require adaptation to local contexts.
8.3 Health Equity and Social Determinants
Addressing social factors is integral to improving overall health and reducing costs.
8.4 Sustainability and Environmental Impact
Healthcare organizations are increasingly adopting eco-friendly practices and sustainable operations.
8.5 Personalization and Consumer-Centric Models
Patients expect tailored experiences, data privacy, and transparency.
Conclusion
The business of healthcare is a complex, dynamic system driven by economic, technological, demographic, and policy forces. It encompasses a broad array of stakeholders, each with unique motivations and challenges. As innovations continue and societal needs evolve, healthcare organizations must adapt strategically to deliver high-quality, efficient, and equitable care while maintaining financial sustainability. Understanding these multifaceted business aspects is essential for policymakers, providers, payers, and innovators dedicated to shaping the future of health and well-being.